Welcome back! Last week, we talked about a very hard-to-talk-about subject. A disease called EB causes infants to have such serious skin breakdown as to result in their death before the age of one. If you missed that blog and would like to catch up, click HERE.
This week, we will tackle a rare disease that affects women more than men. Lupus. What is it, how do we catch it, how do we diagnose, treat, or even cure it? Let’s chat…
Approximately 1.5 million Americans have a form of lupus. Systemic lupus erythematosus cases: 70% of total lupus cases. Of individuals diagnosed with lupus, 90% are women. Eighty percent of people develop lupus between 15 and 45 years of age. A full nine out of ten lupus patients are women. The disease takes many forms and its symptoms vary considerably from one individual to another. Other populations particularly affected are West Indians and African-Americans’.
What is Lupus?
Lupus is a chronic (lifelong) autoimmune disease that can damage any part of the body. With autoimmune diseases, the body’s immune (defense) system cannot tell the difference between viruses, bacteria, and other germs and the body’s healthy cells, tissues, or organs.

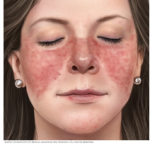
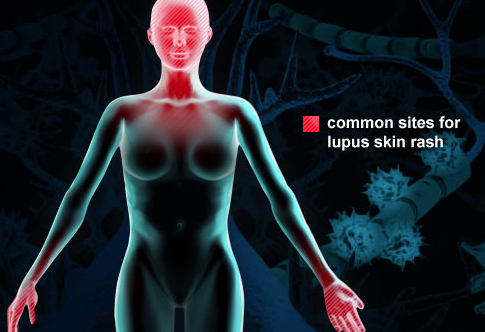
Inflammation caused by lupus can affect many different body systems — including your joints, skin, kidneys, blood cells, brain, heart and lungs. While difficult to diagnose because it’s symptoms also mimic those of other diseases, Lupus tends to have a distinctive sign — a facial rash that resembles the wings of a butterfly unfolding across both cheeks. This occurs in many but not all cases of lupus.
What causes Lupus and is it curable?
Some people are born with a tendency toward developing lupus, which may be triggered by infections, certain drugs or even sunlight. While there’s no cure for lupus, treatments can help control symptoms.
If you are born with an inherited predisposition for lupus, then you may develop the disease when you come into contact with something in the environment that can trigger the disease. While the cause in most cases will remain unknown, some potential triggers include:
- Sunlight. Exposure to the sun may bring on lupus skin lesions or trigger an internal response in susceptible people.
- Infections. Having an infection can initiate lupus or cause a relapse in some people.
- Medications. Lupus can be triggered by certain types of blood pressure medications, anti-seizure medications, and antibiotics. People who have drug-induced lupus usually get better when they stop taking the medication. Rarely, symptoms may persist even after the drug is stopped.
What are the symptoms of Lupus?
This is where it gets tricky. No two cases of Lupus are alike. Thus the difficulty in diagnosing. The Mayo Clinic has this to say about the symptoms of Lupus:

“Signs and symptoms may come on suddenly or develop slowly, may be mild or severe, and may be temporary or permanent. Most people with lupus have mild disease characterized by episodes — called flares — when signs and symptoms get worse for a while, then improve or even disappear completely for a time.
“The signs and symptoms of lupus that you experience will depend on which body systems are affected by the disease. The most common signs and symptoms include:
- Fatigue
- Fever
- Joint pain, stiffness, and swelling
- A butterfly-shaped rash on the face that covers the cheeks and bridge of the nose or rashes elsewhere on the body
- Skin lesions that appear or worsen with sun exposure
- Fingers and toes that turn white or blue when exposed to cold or during stressful periods, also known as Raynaud’s.
- Shortness of breath
- Chest pain
- Dry eyes
- Headaches, confusion and memory loss“
Is there a test for Lupus?
No one test can diagnose lupus. The combination of blood and urine tests, signs and symptoms, and physical examination findings leads to the diagnosis.
Laboratory tests
Blood and urine tests may include:
- Complete blood count. This test measures the number of red blood cells, white blood cells and platelets as well as the amount of hemoglobin, a protein in red blood cells. Results may indicate you have anemia, which commonly occurs in lupus. A low white blood cell or platelet count may occur in lupus as well.
- Erythrocyte sedimentation rate. This blood test determines the rate at which red blood cells settle to the bottom of a tube in an hour. A faster than normal rate may indicate a systemic disease, such as lupus. The sedimentation rate isn’t specific for any one disease. It may be elevated if you have lupus, an infection, another inflammatory condition or cancer.
- Kidney and liver assessment. Blood tests can assess how well your kidneys and liver are functioning. Lupus can affect these organs.
- Urinalysis. An examination of a sample of your urine may show an increased protein level or red blood cells in the urine, which may occur if lupus has affected your kidneys.
- Antinuclear antibody (ANA) test. A positive test for the presence of these antibodies — produced by your immune system — indicates a stimulated immune system. While most people with lupus have a positive ANA test, most people with a positive ANA do not have lupus. If you test positive for ANA, your doctor may advise more-specific antibody testing.
Imaging tests
If your doctor suspects that lupus is affecting your lungs or heart, he or she may suggest:
- Chest X-ray. An image of your chest may reveal abnormal shadows that suggest fluid or inflammation in your lungs.
- Echocardiogram. This test uses sound waves to produce real-time images of your beating heart. It can check for problems with your valves and other portions of your heart.
Biopsy
Lupus can harm your kidneys in many different ways, and treatments can vary, depending on the type of damage that occurs. In some cases, it’s necessary to test a small sample of kidney tissue to determine what the best treatment might be. The sample can be obtained with a needle or through a small incision.
Skin biopsy is sometimes performed to confirm a diagnosis of lupus affecting the skin.
Are there any treatments for Lupus?
Treatment for lupus depends on your signs and symptoms. Determining whether you should be treated and what medications to use requires a careful discussion of the benefits and risks with your doctor.
The medications most commonly used to control lupus include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter NSAIDs, such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others), may be used to treat pain, swelling and fever associated with lupus. Stronger NSAIDs are available by prescription. Side effects of NSAIDs may include stomach bleeding, kidney problems, and an increased risk of heart problems.
- Antimalarial drugs. Medications commonly used to treat malaria, such as hydroxychloroquine (Plaquenil), affect the immune system and can help decrease the risk of lupus flares. Side effects can include stomach upset and, very rarely, damage to the retina of the eye. Regular eye exams are recommended when taking these medications.
- Corticosteroids. Prednisone and other types of corticosteroids can counter the inflammation of lupus. High doses of steroids such as methylprednisolone (Medrol) are often used to control serious disease that involves the kidneys and brain. Side effects include weight gain, easy bruising, thinning bones, high blood pressure, diabetes, and increased risk of infection. The risk of side effects increases with higher doses and longer-term therapy.
- Immunosuppressants. Drugs that suppress the immune system may be helpful in serious cases of lupus. Examples include azathioprine (Imuran, Azasan), mycophenolate (Cellcept), methotrexate (Trexall, Xatmep, others), cyclosporine (Sandimmune, Neoral, Gengraf), and leflunomide (Arava). Potential side effects may include an increased risk of infection, liver damage, decreased fertility, and an increased risk of cancer.
- Biologics. A different type of medication, belimumab (Benlysta) administered intravenously, also reduces lupus symptoms in some people. Side effects include nausea, diarrhea and infections. Rarely, worsening of depression can occur. Rituximab (Rituxan, Truxima) may be beneficial for some people in whom other medications haven’t helped. Side effects include allergic reaction to the intravenous infusion and infections.
What kind of doctor treats Lupus?
A rheumatologist is the specialist who will treat your Lupus symptoms.
If you or someone you know appears to have this rare disease, please consult with a doctor. This blog is not a replacement for sound medical advice, and many diseases, disorders, and syndromes have symptoms that overlap. Only a physician can diagnose you. That said, if you think this blog may be helpful to others, please hit the Facebook Icon and share it on your personal pages. Thank you for reading us, we really do appreciate you!
Thank you for these discussions.
You are very welcome..