Welcome back! Last week we talked about Lyme Disease. If you missed that blog and would like to catch up, click HERE.
This week, by special request from a Junction City Dear Reader, we tackle Hyperhidrosis (hi-pur-hi-DROE-sis).
Hyperhidrosis is defined by the Mayo Clinic as “abnormally excessive sweating that’s not necessarily related to heat or exercise. You may sweat so much that it soaks through your clothes or drips off your hands. Besides disrupting normal daily activities, this type of heavy sweating can cause social anxiety and embarrassment.“
Have you ever met someone who sweats profusely for what appears to be “no reason“? Did you suspect they had something to hide? Were using drugs and needing a “fix“? I would encourage you to consider this blog and the information within before you make a final determination about said person.
The National Organization of Rare Disorders (NORD), states that:
“Primary Hyperhidrosis is a rare disorder that affects males and females in equal numbers. The symptoms of this disorder usually begin during childhood or puberty. Many people with Primary Hyperhidrosis experience relief from the symptoms during adulthood without treatment or obvious reason for the remission.

“Secondary Hyperhidrosis is a more common condition that occurs in association with a variety of other disorders. It is important to distinguish Primary Hyperhidrosis from other underlying disorders that can cause excessive sweating (Secondary Hyperhidrosis). These disorders may include impaired thyroid function, malfunction of the pituitary gland, infectious diseases, diabetes, tumors, gout, menopause, side effects of certain drugs, and/or excessive alcohol consumption“.
Signs and Symptoms:
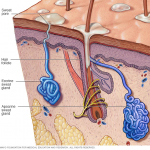
People affected may experience a heightened reaction to certain stimuli that can cause sweating such as anxiety, pain, exercise, tension, caffeine, and/or nicotine. Extreme sweating may occasionally occur all over the body (generalized) or it may be localized in the palms of the hands and the soles of the feet (palmar-plantar hyperhidrosis); the underarm area (axilla); the groin; and under the breasts.
The face may be affected in the form of persistent blushing accompanying the excessive sweating.
When the palms and soles are involved, the skin may develop an abnormal pink or bluish-white appearance. The skin may also become unusually soft (macerated), cracked, or scaly, particularly on the feet.
What Causes this Rare Disorder?
The exact cause of primary hyperhidrosis is not known. The symptoms of this disorder develop due to overactivity of certain sweat glands, and attacks may be precipitated by social and/or physical stress. HOWEVER, even if stress can be identified as the precipitating cause, the disorder does not appear to be the result of a psychiatric disturbance.
Recently, several papers have been published suggesting a genetic origin and transmission of the disorder as an autosomal dominant trait. However, the gene locus has not been identified.
Are there any related disorders?
Yes.
Frey’s Syndrome is a rare neurological disorder that results from injury or surgery near the parotid glands, damaging the facial nerve. The parotid glands are the largest salivary glands in the body and are responsible for the production of saliva. The symptoms of this disorder include flushing and/or sweating on one side of the face. This occurs when hot, spicy, or very acidic foods are consumed.
Greither’s Disease is a rare inherited skin disorder that is characterized by unusual thickness and hardening (keratosis) of the skin on the palms of the hands and soles of the feet. The major symptom of this disorder is excessive sweating of the palms and soles.
A wide variety of conditions can cause profuse sweating as a symptom. These conditions include, but are not limited to: impaired thyroid function, pituitary abnormalities, infectious diseases, vascular obstruction, myasthenia gravis, diabetes, a variety of tumors, gout, menopause, odontoonychodermal dysplasia, dermatopathia pigmentosa reticularis (DPR), Charcot-Marie-Tooth disease type 1, Ross syndrome, Shapiro’s syndrome, Jadassohn-Lewandowsky syndrome, reflex sympathetic dystrophy syndrome, neurogenic acroosteolysis, Weaver syndrome, Gamstorp-Wohlfart syndrome, Meleda disease, Book syndrome, benign essential tremor, blue rubber bleb nevus, pachydermop, and Von Hippel Lindau disease.
How can I get diagnosed?
If you have read this blog and believe that you or someone you know may have this disease, please reach out to your primary care physician. Typically, a Dermatologist is a specialist who can help you with this disorder. This blog is not a replacement for sound medical advice, and many symptoms overlap other diseases, disorders, and syndromes. Only a qualified professional can diagnose you. The diagnosis of primary hyperhidrosis is confirmed by thorough clinical history and evaluation that includes the exclusion of other disorders that may cause excessive sweating.
What is the recommended treatment?
Antiperspirants
People who have mild to moderate primary hyperhidrosis of the palms and soles (Palmar- Plantar type) may find the use of antiperspirants to be effective to some degree. Some physicians recommend aluminum chloride solution 2 to 3 times per week. Wearing cotton socks and canvas shoes and avoiding wool or leather may be of some help as well. The application of medicated powder, formulated to hamper bacterial growth and absorb moisture, may be beneficial in some cases. However, the use of cornstarch is not recommended.

Iontophoresis
The palms and/or soles are immersed in an appropriate electrolyte solution, and a low-intensity electric current (15-18 mA) produced by a DC generator is applied. Treatments last for about 20 minutes and take place regularly several times per week. It has been found effective in some patients with light or moderate disease, but some patients complain of the time taken for treatment and/or expense. The treatment is not applicable to patients with hyperhidrosis of the face or thighs.
Surgical Treatment
For intractable primary hyperhidrosis, surgery may be the treatment of last resort. In general, used is two or three procedures, such as:
Excision (removal) of the axillary sweat glands.
Sympathectomy
The nerves controlling the activity of the sweat glands are part of the sympathetic nervous system that, in turn, is part of the larger system over which people have little or no control, the autonomous nervous system. A surgical procedure that interrupts or redirects the activity of these nerves, such as those dealing with sweating, is called a sympathectomy (the surgical cutting of a sympathetic nerve or removal of a ganglion to relieve a condition affected by its stimulation). In cases of extreme hyperhidrosis, sympathectomy by one or another of several surgical techniques may be selected by the patient. The results of sympathectomy may affect a wide range of sweat glands.
Investigational Therapies
Information on current clinical trials is posted on the Internet at www.clinicaltrials.gov. All studies receiving U.S. government funding, and some supported by private industry, are posted on this government website.
For information about clinical trials being conducted at the National Institutes of Health (NIH) in Bethesda, MD, contact the NIH Patient Recruitment Office:
Tollfree: (800) 411-1222
TTY: (866) 411-1010
Email: prpl@cc.nih.gov
For information about clinical trials sponsored by private sources, contact:
www.centerwatch.com
Please hit the share icon to get this information out to others who may benefit from reading about Hyperhidrosis!
1 Comment