Welcome back! Last week, we researched Antiphospholipid Antibody Syndrome. If you missed that blog and would like to catch up, click HERE.

We had an overwhelmingly positive response to our last two blogs which covered relatively rare disorders, so we’ve decided to dedicate a few new blogs to diseases/syndromes that NORD (National Organization for Rare Disorders) discusses on their web page. This week, we will take a look at Ledderhose Disease.
What is it?
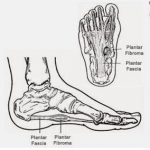
Plantar fascial fibromatosis, also known as Ledderhose’s disease, Morbus Ledderhose, and plantar fibromatosis, is a non-malignant thickening of the deep connective tissue, or fascia, that is found in the arch of the foot. It starts with Plantar Fasciitis, which happens when this area becomes inflamed. The already inflamed tissue develops tumors in the arch of the foot along the length of this band that travels from the heel bone to the toes. In the beginning, when nodules start growing in the fascia of the foot, the disease is minor, but as time wears on it can become so serious as to cause a person to be disabled. The disease got its name from German surgeon Dr. Georg Ledderhose, who first described it in 1894.
How do you pronounce it?
What are the symptoms?
The main symptom is nodules in the arch of the foot, but these nodules can also develop in other areas of the sole of the foot.
Other symptoms include:
- pain in your foot and ankle joints
- tightening of the skin
- pins-and-needles sensation
- Though rare, the thickened skin can pull back on your toes.
- The lumps can sometimes cause the skin to ulcerate from the pressure of rubbing against the socks/shoes/ground.
Is it painful?

Ledderhose Disease takes Plantar Fasciitis (which is very painful) and ramps the pain level up several notches. The inflamed tissue can cause stabbing pain near the heel. Pain is often worse in the morning.
Is it common?
Unlike Plantar Fasciitis, Ledderhose Disease is rather uncommon.
What causes this disease?
Ledderhose disease often affects people with other connective tissue diseases, including Dupuytren’s contracture, and Peyronie’s disease. Up to half of the people with Ledderhose disease also have Dupuytren’s contracture, so it is often assumed they go together, which isn’t always the case.
Though the exact cause of Ledderhose disease isn’t known, both genes and the environment may play roles. The disease is more common in middle-aged and older people, and it occurs much more often in men than in women.
Other factors that may increase your risk of developing Ledderhose include:
- chronic liver disease
- diabetes
- certain medications for epilepsy
- long-term alcohol use
- repeated injuries to your foot
Is there a treatment?
When walking, it’s been described as having rocks in one’s shoes. It is listed as incurable, however, there are soft inserts you can put in your shoes, and also options such as cutting a hole in moleskin to take the pressure off the tumor, but those that live with this disease note that doing this can often make the pain worse.
Other treatments can include physical therapy, massage therapy, shoe inserts, steroid injections, and surgery, however, the doctor I spoke to didn’t recommend surgery for a number of reasons.

The surgery is called fasciectomy. During this procedure, the surgeon will remove part or all of the thickened tissue from your foot. The surgery can leave scars, and Ledderhose disease can eventually come back. Radiation treatment can lower the risk of the disease coming back.
Cryosurgery is another treatment option. Your doctor inserts very cold probes into the lumps to freeze and kill the extra tissue.
A newer treatment uses injections of an enzyme called collagenase to break down the thickened tissue. This treatment is also used for Dupuytren’s contracture.
What type of doctor can treat me?
A podiatrist, also called a doctor of podiatric medicine, is a specialist who provides medical diagnosis and treatment of foot and ankle problems, such as bunions, heel pain, spurs, hammertoes, neuromas, ingrown toenails, warts, corns, and calluses.
Does this disease have a good prognosis?
Treatments can improve the symptoms of Ledderhose disease. Sometimes the condition goes away on its own without treatment.
Less often, the disease gets worse slowly over time. And even when it’s successfully treated, it can come back.
You’re more likely to have a recurrence if any of the following applies:
- You got the disease before age 50.
- You have it in both feet.
- You have a family history of the condition.
- You’re male.
This disease, while very painful, is thankfully very rare. For those living with it, however, that note is of little comfort.
If you found this blog to be helpful, informative, or just a relaxing way to waste time, please do me a favor and share it on your Facebook page? To share, just click on the Facebook icon at the top of this page. Much appreciated!
OMT can also be helpful for symptoms, just so people know 🙂
Reposted from Milwaukie Chit Chat:
Raelynne Virshup
Thanks for sharing. Rare disease day is coming up on 2/28. If you are looking for more topics I have a few rare diseases to suggest. My daughter has a rare disease causing heart defects, lung disease, and her organs to be in incorrect places (heterotaxy). I also work in medically fragile pediatrics as an RN and have met so many amazing folks with rare diseases ??
Reposted from Milwaukie Chit Chat:
Blair Gardner
Love that you are doing this! I can give you lots of interesting rare syndromes and diseases if you are interested. I work at a children’s hospital in Epilepsy. We see many genetic and metabolic disorders.
Reposted from Canby Central:
Jeanette Fanning
I have suffered with this disease for years and did not know the name of this disease. I can now take this article to my Doctor and hopefully get a referral to a podiatrist. Thank you
Thanks for bringing ledderhose disease to the forefront. As a Podiatrist, I have found it difficult to treat but had success recently with injection therapy, orthotics and radiation therapy. My peer review article is due out in the next couple of months on this subject in the American Journal of Podiatric Medicine. Don’t hesitate contacting me with questions at jlmozena@aol.com
I am thrilled! Please let us know when it’s out and we will feature it! Warmly, Linda Tate